COVID-19 has raised the stakes for providers and patients.
In years past, dental providers have generally been adamant about utilizing personal protective equipment and adhering to OSHA and CDC guidance. The onset of COVID-19, however, has raised the stakes for providers and patients. As new safety protocols have emerged, infection control leaders are working hard to keep the industry informed.
Efficiency in Group Practice spoke with training and compliance expert Katherine Schrubbe, RDH, BS, MEd, PhD, about evolving OSHA guidelines and how they will continue to impact dental practices.
Efficiency in Group Practice: How has COVID-19 changed OSHA’s concerns about potential safety hazards in the dental setting?
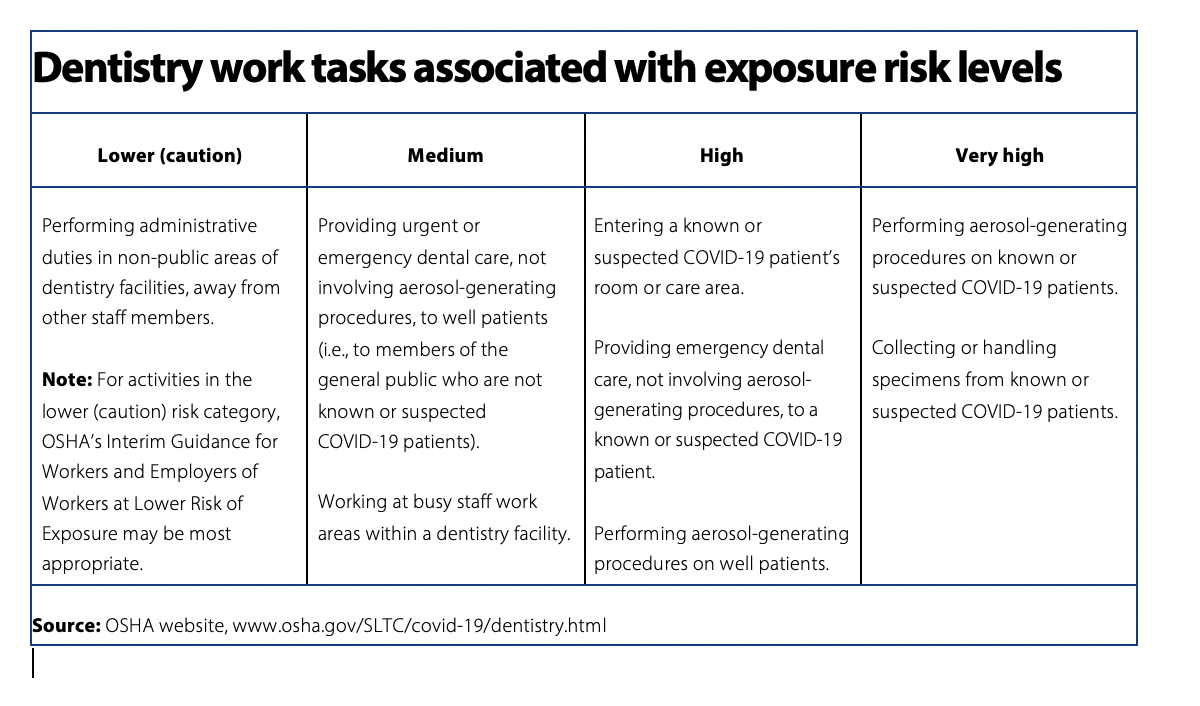
Dr. Katherine Schrubbe: OSHA has issued guidance on COVID-19 for dentistry on a new page entitled Dentistry Workers and Employers. OSHA states that “this guidance is not a standard or regulation, and it creates no new legal obligations. It contains recommendations as well as descriptions of mandatory safety and health standards. The recommendations are advisory in nature, informational in content, and are intended to assist employers in providing a safe and healthful workplace.” (www.osha.gov/SLTC/covid-19/dentistry.html)
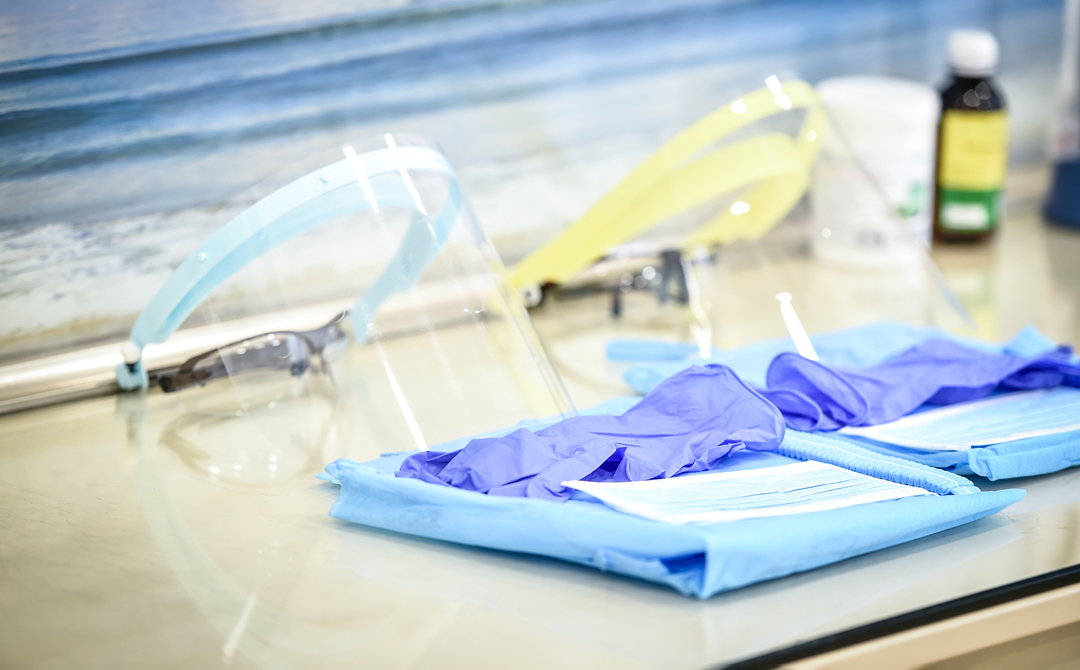
Although dentistry has always dealt with respiratory hazards in the workplace (i.e., spray, spatter and aerosols), SARS-CoV-2 has generated a new level of concern given the high infectivity of the virus and the known risk of droplet transmission, as well as the potential for airborne transmission. Dental providers are the best at utilizing personal protective equipment (PPE) and have been taught to consider every patient infectious; but now they must utilize a higher level of PPE per OSHA and CDC guidance.
On October 5, 2020, the CDC issued an update on their page, How COVID-19 is Spread. According to the update, “under certain conditions, people with COVID-19 seem to have infected others who were more than 6 feet away. These transmissions occurred within enclosed spaces that had inadequate ventilation. Sometimes the infected person was breathing heavily, for example while singing or exercising. Under these circumstances, scientists believe that the amount of infectious smaller droplet and particles produced by the people with COVID-19 became concentrated enough to spread the virus to other people. The people who were infected were in the same space during the same time or shortly after the person with COVID-19 had left. However, available data indicate that it is much more common for the virus that causes COVID-19 to spread through close contact with a person who has COVID-19 than through airborne transmission.” (www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html)
OSHA – as well as the CDC – points out that respirators (NIOSH-certified, disposable N95 filtering facepiece respirator or better) should be worn if dental providers are completing aerosol-generating procedures (AGPs) to ensure the highest level of protection.
Efficiency in Group Practice: Has OSHA changed its approach to conducting inspections, responding to complaints or issuing citations as a result of COVID-19?
Dr. Katherine Schrubbe: This is difficult to say, given that OSHA is a complaint-driven agency and does not have the manpower to check up on every healthcare facility without good cause. However, there seem to be a new crop of OSHA citations and fines related to COVID-19, and many have to do with lack of compliance to the Respiratory Protection Standard, 1910.134. Since the start of the coronavirus pandemic, OSHA has cited 85 establishments for violations, resulting in proposed penalties totaling $1,222,156. (These figures were current at press time and may continue to change. Providers can stay current by visiting https://www.osha.gov/news/newsreleases/national/10022020-0.)
Recent OSHA inspections have resulted in the agency citing employers for a number of violations, including failures to:
- Implement a written respiratory protection program.
- Provide a medical evaluation, respirator fit test, training on the proper use of a respirator, and personal protective equipment.
- Report an injury, illness or fatality.
- Record an injury or illness on OSHA recordkeeping forms.
- Comply with General Duty Clause of the Occupational Safety and Health Act of 1970.
As an example, on September 16, 2020, OSHA cited Georgetown Dental LLC for violating respiratory protection and other standards at the Georgetown, Massachusetts, location. OSHA cited the dental practice for six serious, and one other-than-serious, violations, with proposed penalties totaling $9,500. OSHA cited the dental practice for failing to provide medical evaluations and fit testing for employees required to wear N95 respirators as protection against coronavirus; lack of written programs related to respiratory protection, bloodborne pathogen exposure control and chemical hazard communication; insufficient bloodborne pathogen training and controls; and inadequate eyewash stations.
(https://www.osha.gov/news/newsreleases/national/09162020)
Efficiency in Group Practice: What are the most significant changes dental practices or DSOs have made, as a result of new OSHA guidance and citations?
Dr. Katherine Schrubbe: In my experience, the most significant changes to dental practices and DSOs have been the incorporation of OSHA’s Respiratory Protection Standard and its requirements. If dental providers are utilizing respirators, they need to be worn in the context of the Respiratory Protection Standard. A written plan is now required as part of the practice’s compliance manual, and dental practices must incorporate the various elements of the standard as part of their SOPs, as well as train all team members on this standard and its requirements.
Efficiency in Group Practice: In addition to the coronavirus pandemic, the U.S. continues to experience climate-related disasters, such as hurricanes, flooding and wildfires. Moving forward, how can dental practices better prepare for pandemics or natural disasters?
Dr. Katherine Schrubbe: The United States has had a horrendous 2020 thus far, with wildfires, hurricanes, flooding and a global pandemic. Dental practices have had to step up their compliance to safety guidance very quickly, and many did not plan ahead for extraordinary natural disasters. If this pandemic has taught us anything, it’s that it’s not if, but when, the next thing will happen! That said, there are already tools in place for future planning. OSHA has an excellent webpage on Emergency Preparedness and Response and states, “preparing before an emergency incident plays a vital role in ensuring that employers and workers have the necessary equipment, know where to go, and know how to keep themselves safe when an emergency occurs.” The site addresses how to prepare and train for emergencies, as well as the hazards to be aware of when an emergency occurs, and offers e-tools, fact sheets, quick cards and guidance documents for everything from disease pandemics to nuclear threats. (www.osha.gov/SLTC/emergencypreparedness/)