By Rhonda Mullins
Vital steps to successfully improve case acceptance in group practices
Today’s dental patients are more knowledgeable about the availability and importance of oral health care and those who provide it. It is therefore vital that patients emotionally desire to engage and remain with your practice, but developing that type of relationship involves conveying to patients information that demonstrates the added value and significance that you and your team provide. Case acceptance is impacted greatly by the level of trust, sincerity, expertise and patient care delivery you are perceived to provide, so it is important that it be experienced exceptionally.
Other factors influencing case acceptance are emotional and/or financial uncertainty from the patient or verbal/non-verbal cues from the provider delivering the treatment plan. Your team members may be excellent clinicians but poor communicators. If there is an inability on your team’s part to communicate the necessity of the treatments they are able to provide, it is unlikely they will be given the opportunity to provide them. Additionally, if your team is not able to instill a feeling of trust as the brand insistence for the practice, your patients will be less receptive to being educated throughout the emotional vulnerability or financial uncertainties and fears they are experiencing. Fear is always the backseat driver to perfectionism in achieving optimum outcomes for the patient.
There are ways to ensure your practice is successful at gaining a greater edge in the trust arena with each patient and increased case acceptance. This article outlines vital steps toward obtaining a “yes” from your patients.
Case acceptance begins with a strong internal team
There are three basic types of leadership: laissez-fair; autocratic; and Design Office Collaborator. Laissez-fair is a French term that essentially means “hands-off” in terms of management styles. It implies that the leader – in this case, the practice owner/manager – feels their team is capable of completing all duties with minimal or no direction.1 Autonomy is good, but too much can cause a lack of procedural protocol, which leads to an inefficient practice.1
Autocratic leadership is basically the opposite. The leader assumes their team is incapable of completing their duties without detailed instructions, and the leader’s way is the only right way of doing things.1 This causes team members to feel devalued, which decreases morale and, as a result, cooperation and commitment to the practice. The inefficiencies of this leadership style are caused by denying the viability of other’s opinions or ideas, which may halt progress or even keep the practice from adopting innovations that could help them increase profits and provide higher-level care.
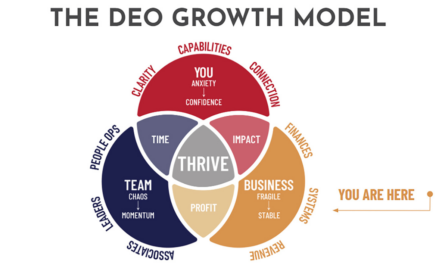
Design Office Collaborator (DOC) leadership is the style best suited to Care Driven® group practices. Leaders who understand this transformative role of design thinking and collaboration in the culture of their office embrace its traits and tenets. They can command in times of change. We call these leaders DOCs, and they are our new heroes.
When we think about design, our first association is change: change that responds to need embodies desire, pursues a stated direction, and reflects a shared vision. Those who are designers – either through training or by nature – actively engage and support congruency in collaborative change. Historically, design changed “things.” More recently, it’s changed services and interactions. Looking ahead, it will change the dental industry. The strength of a practice led by a design office collaborator leader is dependent upon the creative ideas, innovative thinkers, skills, and goals of all team members and doctors being shared and considered on a platform of equals. When a team member knows their opinions and thoughts are truly being heard, and that their talent and skills are being utilized and optimized, it boosts confidence, performance, and a renewed sense of passion for enhancing the changes of the practice.2
You can use your status as a leader to create a positive atmosphere for your team members. According to job satisfaction surveys, workers leave employers, not the place that employs them.3 Human psychology dictates that emotions or moods are proximal, and that we unintentionally affect those around us. Due to the fact that most waking hours are spent at the workplace, team members will be the most notably affected by the mood of their boss. Be aware of your attitudes and actions and consider the effect they will have on the rest of the team.4 Build a strong relationship with your team based on trust and credibility,5 and demonstrate integrity in all situations in your practice: morally; ethically; and honestly.6 Once your leadership and team have coalesced, you are ready to implement the Care Driven® approach in your practice.
Contact
Step one is making meaningful contact and beginning to establishing a relationship with the patient. Multidisciplinary practices accomplish this through a Concierge Extraordinaire. Hire or appoint one or two top-line team members to handle these responsibilities (see Concierge Extraordinaire Responsibilities). Your Concierge must also be certain that patients know what to expect, or how to prepare for, an extraordinary experience with a comfortable, open atmosphere during future appointments. The Concierge’s thorough Pre-appointment Discovery meeting with the patient provides useful information for the team, but also builds relationship equity with the practice from the very beginning.
Clarity
Step two is creating a value proposition opportunity to learn more about any patient and where they are in terms of medical, emotional, clinical and financial status. Using supporting technology that the patient experiences with the Concierge as a guide, conduct an inner-view verses an interview in which you engage in open-ended questions. These should invite patients to talk about their needs, wants, and life circumstances and what led them to desire your expertise and care. This will ensure that the answer you receive in the end is a “yes” to your case synopsis treatment recommendations for their desired outcome.
This is also the time to tailor your strategy for interacting with patients based on whether they are new to the practice, an emergency patient, or an existing patient. The new patient approach is discovery-driven. For this type of patient, you and your team are gathering information about their overall and oral health, as well as their esthetic goals. Do they desire to re-create a smile they had or design a new smile? Listen intently to their words, and watch their face and body language for reactions. The more the patient says and you hear, and the more the patient does that you observe and record, the more thorough your data collection will be. Accurate and complete notes will provide a better basis for the multi-disciplinary doctors and team members’ clarity about the patient and their needs.
The emergency patient approach is need-driven. These patients have an immediate treatment that must occur, after which the new patient approach can be implemented. The existing patient approach is maintenance-based. This type of patient will have a comprehensive treatment plan in place, but in the event a trauma or other changes occur, they may need sequencing modifications or updated treatment recommendations. If this occurs, take them through the new patient approach and anticipate optimum results based on their continued care behavior and updated treatment plan.
All three types require a baseline record and risk-assessment performed that include medical and dental history forms, a question and answer session, X-rays, camera/digital/CEREC images, intraoral/extraoral imaging, oral cancer screening, models (face-bow, etc.,) and risk assessment checkpoints and documentation (see Risk Assessment:Checkpoints and Documentation).
Create risk assessment, care plan, and present
Step three is presentation of your Multi-Disciplinary Team Approach and detailed treatment recommendations to the patient. It is important that top-line internal team members engage at the touch-point moment (especially the financial facilitator) at the diagnosis’s. You will need to outline the specific direction and process necessary to deliver the best results possible. If you consistently under-promise and over-perform, then the patient’s transformation will appear much more measurable to them, since you will have delivered a higher level of care than expected. You can deliver optimum results to your patients in the four areas of oral health that you and your team assessed for risk: periodontal; biochemical; functional; and dentofacial (see Optimum Outcome Treatment Options). By clearly explaining the available treatment options and their benefits, realistic expectations can be established for a well-delivered Care Driven® plan.
Commit
During step four, present your Care Driven® plans (one or two), including financial investment. A Care Driven® plan not only increases your patient’s understanding of what is involved in their transformation, but also enhances their understanding of how this transformation is an investment in their present and future health.
This is the integral conversion moment and value proposition. Your patient’s decision about whether or not to proceed with treatment will ultimately rest in the hands of their emotions, not their finances. That is why it is paramount at this stage to promote the value-added benefits of your brand, reputation, and expertise that this transformation will provide, such as greater self-worth, confidence, and whole-heartedness. This will lead them to greater achievement and success. Patients will find money for treatments they want, but may find excuses to delay treatments they need. After hearing and processing all the information you and your team have presented, your financial facilitator and concierge will be able to walk the patient through the rest of the process (see Financial Facilitator/Concierge Role in Patient Commitment).
Care Driven® Appointment Sequencing
Step five involves scheduling each patient’s appointments in a prescribed manner according to:
- Concierge Extraordinaire Touch Plan (Introduction and Interview)
- Care Driven® Risk Assessment and Care Driven® Plan
- Multi-Disciplinary Team / Specialists
- Re-appointments
- Active Care Completion
- Post-activity Re-assessment (Metrics)
- Case Completion
- Maintenance and Preventative Care
The Care Driven® approach is superior to other practice models because the patient feels seen and heard, efficiently cared for, and valued, which positively affects the practice. There is an increased attendance to follow-up, hygiene, and maintenance appointments. More patients refer their friends and family because they feel it is a creative culture for care. Treatment acceptance increases because patients trust and value in a greater capacity what the practice is providing and do not feel as though they are being pressured through proceedings. Additionally, unlike the way some practices undertake the maintenance care of completed cases using a “clean and screen” method, Care Driven® practices see this as yet another opportunity to provide above-and-beyond total care to the patient, ensuring they feel satisfied with their transformation both emotionally and physically.
A better patient experience
Patients demand the best available treatments and want to feel truly cared for in their chosen dental practice. When patients choose a Care Driven® multidisciplinary practice, they should know from the first phone call or meeting with the Concierge Extraordinaire that they can expect a better experience throughout their treatments and maintenance care.
The core of attaining increased case acceptance is presenting like a professional. This is accomplished through Design Office Collaborators (DOC) best suited to a Care Driven® group practice. Remember, these leaders understand this transformative role throughout these 5 steps of engagement because of design thinking and collaboration with each patient’s individual needs. They are tomorrow’s new heroes in group practices.
You and your Multi-Disciplinary Specialist Team must demonstrate exemplary clinical aptitude and relationship investment in your patient’s well being. This is especially important because patients base decisions more on emotion and desire than on how effectively information has been conveyed to them. This Care Driven® Plan strategy is most effectively implemented after completion of the Kois Center Treatment Planning Course I.7
References
- Goodnight R. Laissez-fair leadership. Encyclopedia of Leadership. Sage Publications. 2004;820-823.
- Eisenberger R, Cummings J, Armeli S, Lynch P. Perceived organizational support, discretionary treatment, and job satisfaction. Journal of Applied Psych. 1997;82(5):812-820.
- Gardner M. Seven things employees want most to be happy at work. The Christian Science Monitor, 2008. www.csmonitor.com/Business/2008/0128/p13s03-wmgn.html. Accessed September 26, 2013.
- Goleman D, Boyatzis R, McKee A. Primal leadership: the hidden driver of great performance. Harvard Business Review. 2001;79(11):41-51.
- Budd JF Jr. The incredible incredibility dilemma: credibility in public relations. Public Relations Quarterly. October 1, 2000. http://www.highbeam.com/doc/1P3-63356286.html. Accessed September 27, 2013.
- Leadership credibility why is it so important? Leader Today. http://leadertoday.org/faq/credibility.htm. Accessed September 26, 2013.
- Kois Center. Kois center treatment planning course I: course overview. http://koiscenter.com/store/course_overview.aspx?id=22. Accessed September 25, 2013
Sidebar: Optimum Outcome Treatment Options
Periodontal
- Maintenance Interval
- Extraction
- Surgical Correction
- Orthodontic Correction
- Other
- Multi-Disciplinary Specialist Referral
Biochemical
- Alloys
- Composites
- Root Canal Therapy
- Foundation Requirements
- Other
- Multi-Disciplinary Specialist Referral
Functional
- Occlusal Adjustment/Contour/Alteration/Appliance Therapy
- Extraction
- TMJ Stabilization
- Surgical
- Orthodontic
- Periodontal
Dentofacial
- Color of Smile
- Facially-related Tooth Position
- Intra-arch Tooth Position
- Gingival Tissue Assessment Results
Sidebar: Financial Facilitator/Concierge Role in Patient Commitment
- Be the bridge of communication working with the patient for and among all doctors and team members.
- Know how to ask for feedback from patients about their Care Driven® plans to enhance their optimum results.
- Recognize and offer workable solutions to patient barriers (financial, emotional, etc.).
- Assist the patient through the full process of obtaining third-party financing or understanding and fully utilizing their insurance benefits.
Sidebar:
Risk Assessment: Checkpoints and Documentation
- Periodontal Assessment
- Gingival
- Attachment Loss
- Restoration Enhancement
Biochemical Assessment
- Determine Restoration Design
Functional Assessment (involves teeth, joints, and musculature)
- Control
- Comfort
- Stabilization
Dentofacial Assessment
- Tooth Display
- Tooth Position
- Gingival Architecture
Sidebar:
Concierge Extraordinaire Responsibilities
- Set the tone for expectations of care and exceeding those expectations.
- Tell the patient who will greet them and what they will experience at their first reserved appointment.
- Listen carefully and document all of the patient’s previous experiences, expectations, fears, etc. and extract the specific information that will allow the entire team to over-anticipate patient needs.
- Walk the patient through completion of all paperwork and why it is needed.
- Offer website for directions and confirm date and time of the next appointment.
- Share the doctor’s standards, education, qualifications, training, and passions to instill confidence that the right choice in practices has been made by the patient.